Drug-resistant bacteria add another layer to India’s coronavirus battle
09/20/2021 / By Ramon Tomey
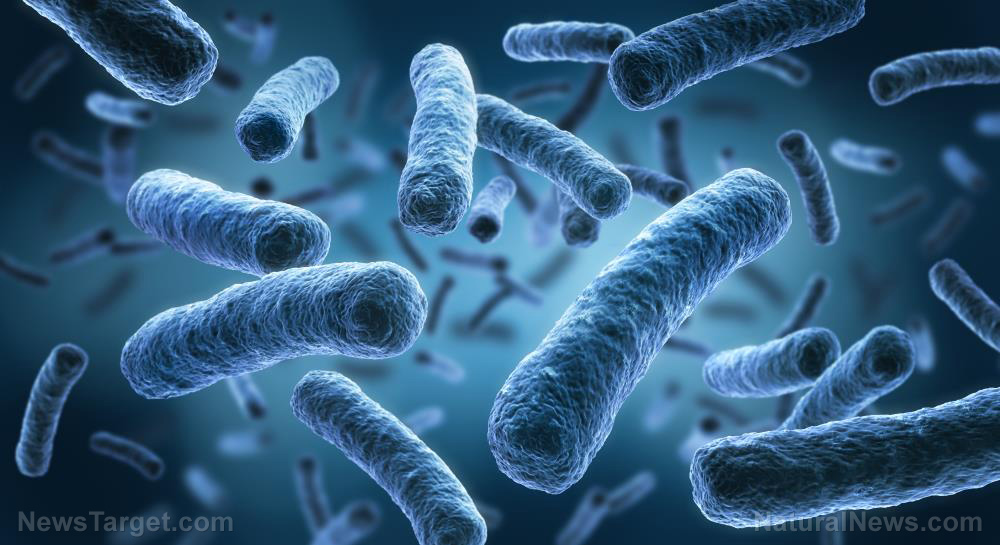
A majority of doctors in India say they would prescribe high doses of potent antibiotics to patients for different kinds of diseases, causing the rise of drug-resistant strains. The Wuhan coronavirus (COVID-19) pandemic revealed many hospitalized patients during the first wave with bacterial and fungal infections that antibiotics seemingly cannot cure. This added an extra layer of difficulty for health workers that now have to deal with both SARS-CoV-2 and the drug-resistant pathogens.
Indian Council of Medical Research (ICMR) microbiologist Kamini Walia pointed out that the overuse of potent antibiotics may be “adding fuel to the fire of the already alarming antimicrobial resistance levels. These potent antibiotics included some medications reserved for the cases hardest to treat.
“Fear of missing a secondary infection and lack of specific therapy for COVID-19 leads to over-prescription of antibiotics,” she said. Walia added: “The culture of over-medicating through antibiotics predates the pandemic.”
She noted that doctors had a tendency to prescribe three or four antibiotics to intensive care patients while waiting for lab results that determine the need for the drugs. This was often done to “plug the gaps” in infection control and prevention. Walia explained: “Antimicrobials are a shield, and as long as the patient is feeling better, doctors don’t want to de-escalate the antibiotic regimen. And the price for that comes three to six months down the line.”
According to the World Health Organization (WHO), antibiotic resistance is one of the biggest threats to global health, food security and development. The global health body said: “New resistance mechanisms are emerging and spreading globally, threatening our ability to treat common infectious diseases. A growing list of infections … are becoming harder, and sometimes impossible, to treat as antibiotics become less effective.” (Related: Loose regulatory action in India continues to allow production of unapproved antibiotic formulas.)
Drug-resistant pathogens have been found in coronavirus-positive Indians
Walia and her colleagues penned a study that looked at secondary infections in COVID-19 patients, which was subsequently published in Infection and Drug Resistance in May 2021. They examined data from 17,534 patients admitted in any of the 10 hospitals part of the IMCR’s surveillance network from June 1 to Aug. 30 of last year.
Of the more than 17,000 patients, 3.6 percent or 640 patients contracted a secondary infection. However, the researchers noted that some hospitals registered secondary infection rates as high as 28 percent. Pathogens that resisted multiple drugs caused co-infections in about half of the cases.
Meanwhile, almost 60 percent of patients with secondary infections died. Only 11 percent of those who did not pick up another pathogen died, the study said. Majority of patients who died had conditions that exacerbated COVID-19 such as diabetes or hypertension. New Delhi-based Center for Disease Dynamics, Economics and Policy Director Dr. Ramanan Laxminarayan said of the study: “It shows that if [COVID-19] doesn’t kill you, these secondary infections can.”
Walia and her colleagues found that many Indians who contracted COVID-19 were prescribed strong antibiotics for their predicament. These drugs included the most potent antibacterial carbapenem and colistin, a “drug of last resort” typically reserved for the most stubborn strains. They noted that pathogens such as Klebsiella pneumoniae and Acinetobacter baumannii resisting these potent antibiotics was “an alarming finding.”
The researchers added that the use of steroids that weakened the immune system also played a role in the occurrence of secondary infections. Steroids were used mainly to subdue the inflammations accompanying COVID-19 at the cost of undermined immunity. This subsequently triggered cases of a fungal infection called mucormycosis.
Mumbai-based eye surgeon Dr. Akshay Nair said the fungus responsible for mucormycosis was ubiquitous. “It … [is] found in soil, [in] air and even in the nose and mucus of healthy people,” he told the BBC‘s Soutik Biswas. (Related: Deadly “black fungus” infection spreads among coronavirus patients in India.)
Laxminarayan remarked: “Early steroid use tends to tamp down the body’s immunity, leaving it more vulnerable to other infections.” He ultimately warned that the indiscriminate use of antibiotics and steroids is as detrimental as the disease they are targeting and that it “is going to haunt India in the months to come.”
Visit Pandemic.news to read more stories about India’s battle against COVID-19 and drug-resistant bacteria.
Sources include:
Tagged Under: antibiotic drugs, antibiotic misuse, Antibiotics, covid-19 pandemic, drug-resistant bacteria, immune system, India, inflammation, mucormycosis, secondary infection, steroid use, superbugs, weakened immunity, Wuhan coronavirus
RECENT NEWS & ARTICLES
ImmuneSystem.News is a fact-based public education website published by Immune System News Features, LLC.
All content copyright © 2018 by Immune System News Features, LLC.
Contact Us with Tips or Corrections
All trademarks, registered trademarks and servicemarks mentioned on this site are the property of their respective owners.